In Vitro Diagnostic Devices Regulation
The IVDR EU Regulation 2017/746 is – like the name already implies – related to In Vitro Diagnostic Medical Devices. This European regulation has come into effect on May 26, 2022 to guarantee the smooth functioning of internal markets for In Vitro Diagnostic Devices by establishing a robust, transparent, predictable, and sustainable regulatory framework that supports innovation. The IVDR repeals and replaces IVDD 98/97/EC directive and is widely considered to be more comprehensive than its predecessor.
IVDR Classification of Devices
An essential aspect of the IVDR is that it recommends a rule-based device classification system in Annex VIII. The rule-based classification system is based on patient-risk severity and contains four classes:
Class A: Low patient and public health risk
This could for example be a buffer solution for the in vitro diagnostics of a specific disease condition. Class A includes accessories that possess no critical characteristics, and chemicals or biomaterials such as buffer solutions, washing solutions, culture media, and histological stains.
Class B: Moderate patient risk and/or low public health risk
Examples of this class are devices for fertility testing, determining cholesterol levels, and devices for detecting pregnancy as well as detecting glucose, erythrocytes, leucocytes, and bacteria in the urine.
Class C: High patient risk and/or moderate public health risk
Devices used for identifying blood group, tissue type to examine the immunological compatibility of blood, blood components, cells, tissue fall in this class. Similarly, organs intended for the purpose of transfusion or transplantation, or cell administration, are classified as class C.
Class D: High patient risk and high public health risk
An example of a class D device would be a device for detecting the presence or exposure to a transmissible agent that causes a life-threatening disease with a high – or suspected to be high – risk of propagation.
The correct classification of an IVD device is essential, as the regulatory compliance requirements are high for classes with high patient and public health risks compared to classes with low risks. For example, all IVD device classes other than Class A and non-sterile devices will be audited annually by a Notified Body (NB) to ensure compliance with IVDR classification and other applicable requirements. Additionally, only manufacturers of class A and non-sterile devices will be able to self-certify their products. Therefore, almost 80%-90% of IVD devices will have to undergo a compliance check by an NB before receiving their CE mark, which is mandatory to enter major markets.
IVDR Process Steps
IVD devices will generally pass through the following steps to demonstrate their compliance with the IVDR:
- Appointing a European Authorized Representative.
- Identifying applicable EU directives and regulations.
- Deciding and performing appropriate conformity assessment procedures.
- Checking the device against the general safety and performance requirements listed in Annex I.
- Identifying applicable harmonized standards for the device.
- Preparing a technical file as described in Annex II and Annex III, and implementing the quality management system.
- Selecting an NB (except for class A) and signing the declaration of conformity.
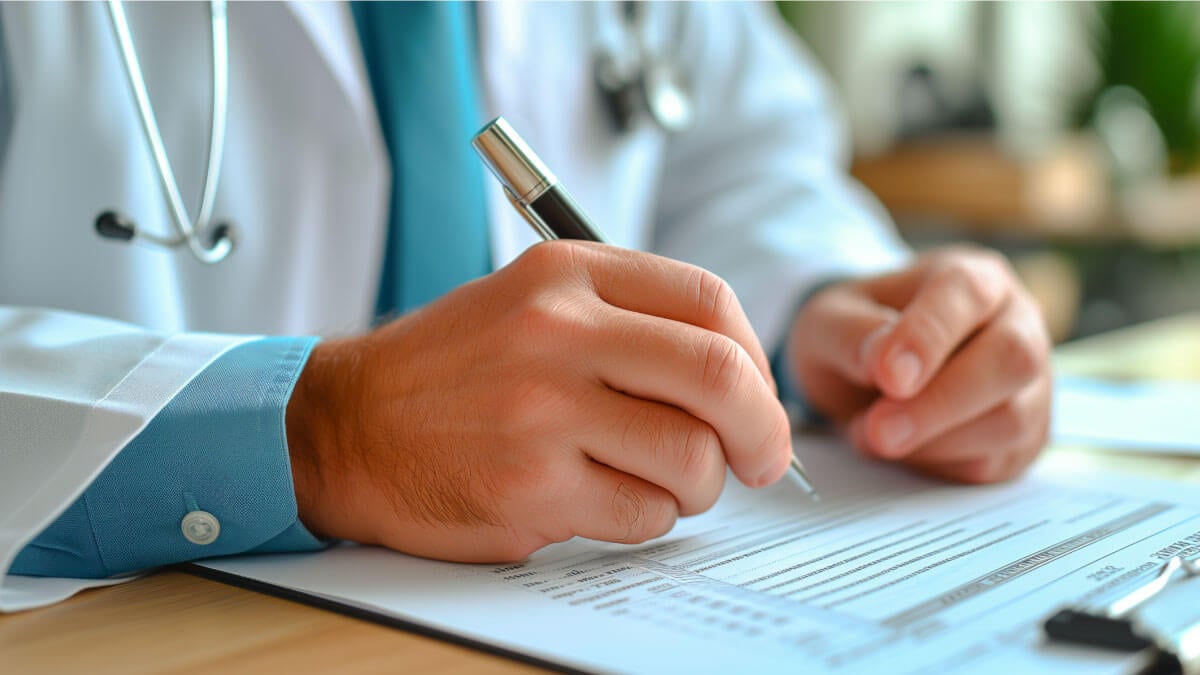
IVDR Post Market Surveillance
Post Marketing Surveillance (PMS) is a comprehensive process for monitoring and assessing the safety and performance of IVD devices. Although it is named ‘post-marketing,’ in practice, it begins long before the device becomes available on the European market and even continues for the entire lifecycle of the device. Despite its name, PMS is an ongoing process, not a one-time project. An effective and IVDR-compliant PMS must:
- Be scheduled regularly,
- Actively record complaints, and
- Be well-documented to report all processes and results.
As stated above, NBs must conduct audits at least every 12 months (except for class A devices and non-sterile products). Such annual audits include assessing PMS planning, data analysis, and reporting. Simply put, manufacturers “must do what they say” by following the three points we stated above.
In addition to the annual audits, NBs are required to conduct surprise audits at least once every five years.
Understandably, the extent of PMS activities is dependent on the risk associated with the device. PMS activities related to a low-risk Class A device will differ from those for a high-risk Class D device. In addition to the extent of the activities, data collection requirements also vary by IVD class. Annex A of ISO/TR 20416:2020 includes numerous examples of proactive data sources for active PMS. Manufacturers need to document all market surveillance activities, and NBs review all documented activities during annual surveillance audits. Manufacturers cannot just wait for complaints as a passive approach to the IVDR.
Additional resources

How to Implement the Continuous Improvement Cycle | Scilife
Even an organization with stellar leadership and a solid core of employees experiences hiccups from time to time. Despite having assembled all the ...
How to assess and enhance your Quality Management Maturity | Scilife
As the life sciences industry becomes increasingly regulated and competitive, quality management has become more vital than ever. Are you confident ...
Best Quality Management Software (QMS) for Life Sciences | Scilife
The right electronic Quality Management System (eQMS) can help strengthen your compliance processes and build a culture of quality within your ...
How to write a good quality plan for medical devices | Scilife
In life sciences, especially if you’re in the medical device industry it becomes harder to manage projects in accordance with your company’s quality ...
Turn quality into your brightest asset with Scilife
